What is a stroke?
A stroke is when the blood flow to the brain stops. A stroke is a medical emergency. Call 9-1-1 right away if you think that you or someone you know is having a stroke. It is important to get to a hospital fast so doctors can treat the stroke while it is happening.
What is a TIA?
TIA stands for transient ischemic attack. TIA is also known as a mini-stroke or a warning stroke. TIA happens when there is brief blockage of blood flow to the brain. TIAs usually last less than 5 minutes and should not be ignored. Call 9-1-1 and get medical help right away. They often are a sign that the person is at risk of having a full stroke with much more serious consequences.
MaineHealth Telestroke Network
Through the MaineHealth Telestroke Network, our neurovascular experts provide emergency consultations for stroke patients 24/7. We bring the expertise of top neurologists to community hospital emergency departments, when it is needed most. Using state-of-the-art video conferencing equipment and electronic transfer of CT scans, the TeleStroke network gives community-based physicians timely access to consultations from specialists skilled in the diagnosis and treatment of stroke patients. Participating hospitals include:
For more information about the TeleStroke network, please contact Brian Chipman RN, BSN at brian.chipman@mainehealth.org.
More about Strokes
Stroke Symptoms
The following may be signs and symptoms of a stroke. Call 9-1-1 or seek emergency medical care right away if you or someone you know has any of the following symptoms:
- One side of their face is drooping or feels numb.
- One arm feels weak or numb.
- One side of the body feels weak or numb.
- Loss of balance, or feeling dizzy.
- Sudden severe headache.
- Trouble seeing out of 1 or both eyes.
- Trouble speaking, unable to talk, hard to understand, or having a hard time finding the right words.
The American Stroke Association recommends using the FAST acronym to identify signs of a stroke.
F: Face drooping
A: Arm weakness
S: Speech changes
T: Time to call 9-1-1
Get Help Right Away
It is very important to get medical care right away if you or someone you know is having a stroke. Early treatment will improve the chances of a full recovery. Call 9-1-1 right away if you think someone is having a stroke.Tests Done in the Emergency Department
When someone who may be having a stroke arrives in the emergency department, some of these tests may be performed right away to diagnose a stroke:
- CT scan
- CT Angiogram (not angiocardiogram)
- CT Perfusion scan
- EKG
- Blood tests
- MRI
The following tests may be done later on during the hospital stay:
- Carotid ultrasound
- MRA
- CT angiogram
- Carotid angiogram
Fast Treatment is Important
The best treatment for a stroke is to stop it while it is happening. If you are having any stroke symptoms, call 911 and get medical treatment right away. Doctors will need to dissolve or remove the blood clot, or stop the bleeding.
The longer a patient waits for treatment, the more damage there may be to the brain. For this reason, our system works to speed up stroke diagnosis and treatment. As a result of close collaboration between the stroke program, MMC's Emergency Department, and state-wide stroke initiatives, more patients are able to receive stroke care within the three-hour window needed for tPA administration.
Stroke patients may be given a clot-busting drug called tPA or TNK. These are considered to be the gold standard. These drugs help to dissolve the blood clot and improve blood flow to the part of the brain affected by the stroke. These drugs can only be given within a certain time frame, so it is important to get to a hospital as soon as possible.
MMC also offers endovascular stroke treatments to remove the clot by sending a catheter to the site of the blocked blood vessel in the brain. Patients must meet certain criteria to be eligible.
Sometimes these procedures involve the administration of tPA directly into the blood clot (called intra-arterial treatment) to help dissolve the blockage. In other procedures, the doctor may be able to remove the blood clot. Research has shown that certain patients may be eligible for an extended treatment window for this procedure, but never delay emergency medical treatment if stroke is suspected.
An endovascular procedure or mechanical thrombectomy is an option for eligible patients having a stroke in a large vessel in the brain.
After emergency care has been given, treatment options may also include the use of blood thinners; and physical, occupational, and speech therapies.
Stroke Rehabilitation and Therapy
Stroke rehabilitation and therapy help patients recover from damage caused by stroke. Stroke rehabilitation is focused on helping you get back to leading a healthy and active lifestyle. Some members of the rehab team that will help you on this journey include: physiatrist, physical therapist, occupational therapist, speech language pathologist, doctors and nurses.
There are different types of stroke rehab and you will be referred to the type that best matches your needs. Patients often can get stroke therapy services close to home, so there is no need to travel far during stroke recovery.
What are the risk factors for stroke?
These risk factors may increase the chance of having a stroke:
- Age: The likelihood of having a stroke increases with age for both males and females. Although stroke is more common among the elderly, a lot of people under 65 also have strokes. Even babies and children can have a stroke.
- Family history of heart disease
- Family history of sickle cell disease
- Being African American, Native American or Alaskan Native
- Having a previous stroke, TIA or heart attack
- Smoking or being exposed to secondhand smoke
- High blood pressure
- High cholesterol
- Obesity
- Diabetes
- Stress
- Drug or alcohol misuse or abuse
- Inactive lifestyle
Although people cannot change some risk factors for stroke, like age and family history, there are lifestyle changes that can lower the risk for having a stroke. Your doctor can help you make healthy lifestyle changes and connect you with resources to help lower the risk for stroke.
There are some healthy lifestyle changes that can lower your risk for stroke. These lifestyle changes include:
- Lower & manage high blood pressure
- Control cholesterol levels
- Lower blood sugar levels
- Be physically active
- Eat healthy foods
- Maintain a healthy weight
- Limit alcohol
- Quit smoking
- Avoid second-hand smoke
Ask your doctor for help with making these healthy lifestyle changes.
MaineHealth Telestroke Network Performance at a Glance:
- Average consult callback time is 4 minutes
- Patients considered eligible for thrombolytic therapy (clot-busting medicine) at the time of consult request = 46%
- Percentage of eligible patients who receive thrombolytic therapy = 41%
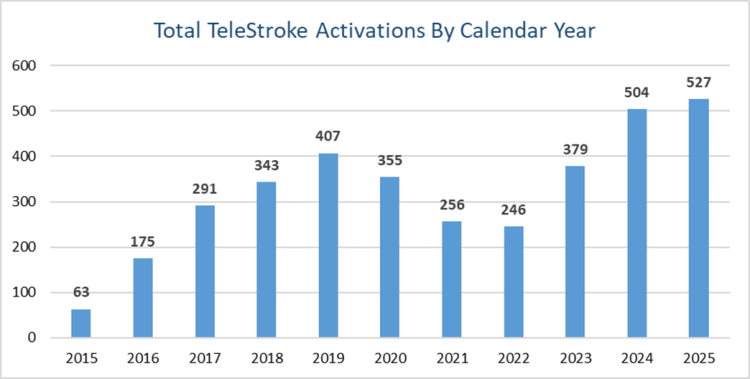
Telestroke consults by calendar year since program inception:
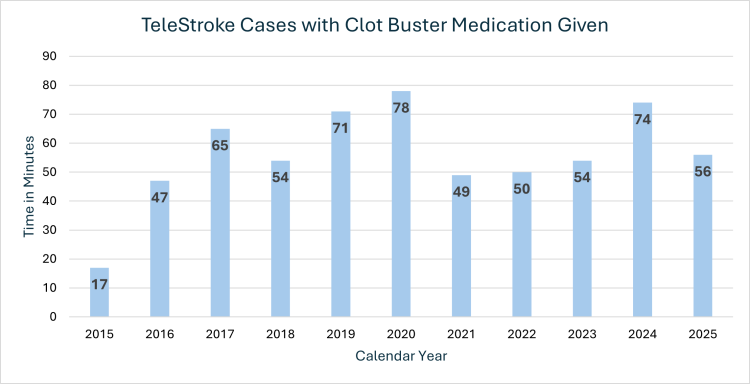
TeleStroke Cases with Clot Buster Medication Given:
Telestroke median door-to-clot buster administered:
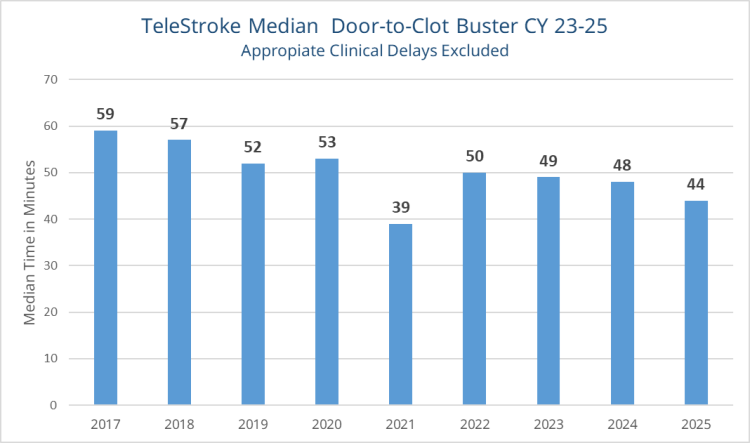
Door to thrombolytic therapy median time:
This graph represents the span of time from arrival at hospital until thrombolytic (clot-busting medicine) is administered. This time span represents the primary benchmark we use to determine the quality of the Telestroke program. The median time goal was reduced in 2019 to 45 minutes from 60 minutes. We continue to show progress toward this goal.

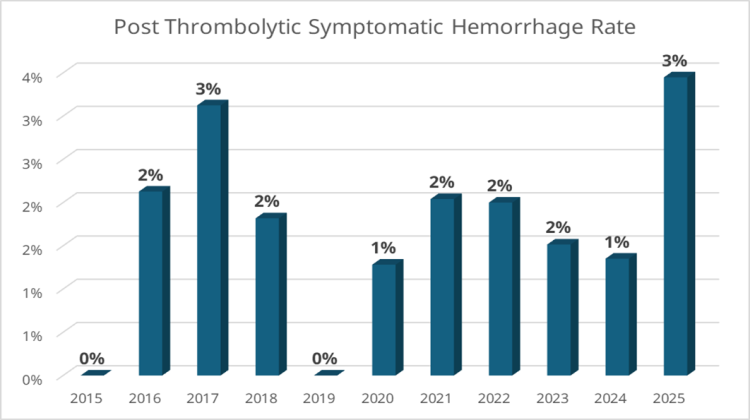
Thrombolytic-associated intracerebral hemorrhage (ICH) for TeleStroke patients:
Complications of thrombolytic therapy include bleeding in the brain, also called intracerebral hemorrhage (ICH). If a stroke patient has post-thrombolytic bleeding in the brain and it makes their condition worse, it is called a symptomatic intracerebral hemorrhage.
Telestroke is a way for specially-trained doctors to evaluate, diagnose, and make a treatment plan for patients at local hospitals where a stroke expert is not available. A telestroke consultation uses two-way videoconferencing to connect you, your loved one and your local emergency department (ED) care team with a stroke expert at another hospital.
Why is telestroke helpful in stroke care?
A stroke is an time-sensitive medical emergency. Every minute that circulation is obstructed to a portion of the brain results in 1.9 million neurons (brain cells) lost. If you are having a stroke, you need to be seen right away by a medical provider who specializes in stroke treatment. Many local hospitals do not have stroke experts on site but your local ED care team can work with a stroke expert from a different hospital through a telestroke consultation. Access to specialists via telestroke reduces the time to treatment decision, thereby saving brain cells. And, hospitals that participate in the telestroke program have shown improvement in time to treatment, potentially saving neurons.
Did you know? Stroke is the leading cause of long-term disability in the US, costing an estimated $34 billion each year.
What is a telestroke consultation?
The stroke expert will assess you or your loved one using a two-way teleconferencing system to see and speak with you and your local ED care team. Together they will recommend the best care plan for you or your loved one. Your team may also suggest that you or your loved one should be moved to another hospital for more care.
What are the benefits of telestroke?
Telestroke lets a stroke expert give you care quickly, even if they are not able to be there with you at the hospital. The care given through the telestroke consultation will be the same type of care you would get from a stroke expert in person.
What are the risks of telestroke?
There are no known or expected risks from taking part in a telestroke consultation. The appointment will not be recorded and no photographs will be taken. The information shared during the consultation will be documented in the patient’s medical record.




























